CHC Full Assessment
If the outcome of the Checklist is positive, your relative will progress to a Full Assessment. Often referred to as “the MDT”, the Full Assessment should take place within 28 days of the Checklist.
The Full CHC Assessment is carried out by a Multidisciplinary Team (MDT). To meet the requirements of the National Framework, the MDT must comprise two professionals of different backgrounds and experience. Ideally, this should be one healthcare professional (usually a nurse) and one Social Services professional (usually a social worker), but may sometimes be two nurses of different skillsets (e.g., one general nurse and one mental health nurse).
The MDT members must be properly trained in the National Framework and the assessment process. They should also be knowledgeable about your relative’s health and social care needs and, where possible, have recently been involved in their treatment or care.
The MDT should gather as much information as possible about your relative’s care needs, taking into account relevant medical and care records, and the views of the care team. If there are discrepancies between verbal and written information, the MDT should attempt to resolve these before making a recommendation as to CHC eligibility.
The MDT will be coordinated and chaired by the Nurse Assessor, working for the Integrated Care Board, which is the local arm of the NHS. You should be given plenty of notice of the assessment and be encouraged to participate fully in the process.
We can offer you advocacy support through our MDT Advocacy Service.
CHC Assessment Scoring
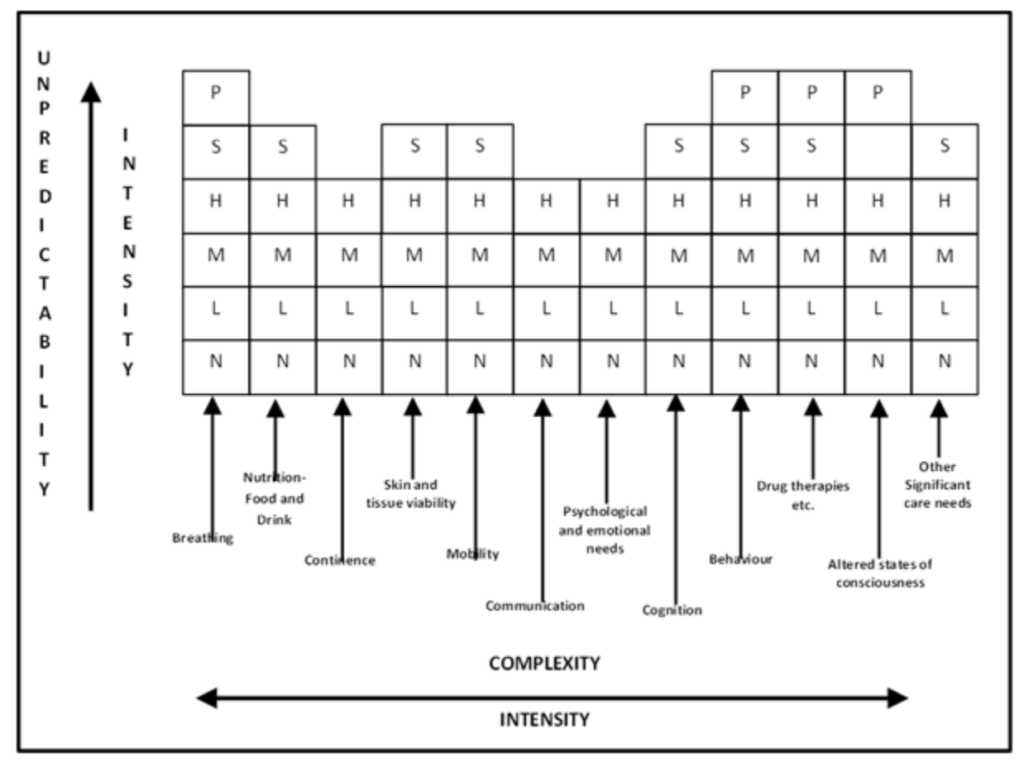
The Full Assessment follows a similar process to the Checklist, but uses a Decision Support Tool (DST) instead. The DST has all the same Care Domains as the Checklist, plus one further Domain for “Other Significant Needs”, which cannot be captured elsewhere.
What is the Decision Support Tool (DST)?
The Decision Support Tool collates relevant information across key areas of care, assisting practitioners in making evidence-led, consistent recommendations.
While the levels of need are only a guide, helping the MDT to assess the totality and interaction of the care interventions, a recommendation of eligibility for NHS CHC Funding is expected if there is evidence of one ‘Priority’ level of need or a ‘Severe’ level of need in two or more domains.
However, it is not necessary to meet this threshold in order to qualify: it is the nature, intensity, complexity and unpredictability of the care needs that determines eligibility. These criteria – called the four “Key Characteristics” – are the “Primary Health Need” test. Once the care domains on the DST have been completed, the MDT applies these criteria, before making a recommendation as to CHC eligibility.
The completed DST and MDT recommendation are then sent to the Integrated Care Board, which makes the final decision.
In most cases, it is expected that the ICB will accept the MDT’s recommendation. However, this is not a given and there are circumstances under which the ICB can reject the recommendation of the MDT. Many ICB’s use a Ratification Panel to make the final decision; this Panel may request further evidence from the MDT or even alter the levels of need.
Once the decision has been ratified, the ICB will send a formal Outcome Letter, enclosing a copy of the final Decision Support Tool. If the outcome is negative, the letter should explain the process and timeframe for appeal.
If you disagree with the ICB’s decision, you can appeal – first to the ICB itself and then to NHS England. The statutory deadline for appeal is 6 months from the date of the Outcome Letter.

Meeting CHC criteria
If your relative is found to meet the criteria for NHS Continuing Healthcare Funding, it is then the responsibility of the NHS to commission and pay for 100% of their care. Being asked to top-up a CHC package is unlawful.
The NHS will conduct a review of the care package after three months to see whether it remains appropriate. If there has been a significant change in need, a further Full Assessment will be undertaken, at which point your relative’s funding may be withdrawn.
You should be informed of any upcoming review and invited to participate. Don’t be complacent – make sure you prepare as you would for a Full Assessment, to minimize the chances of CHC being removed.
If nothing has changed at the 3-month review, CHC will simply continue. Reviews will then be undertaken annually. Again, it is important to attend these reviews to ensure they are conducted properly.
Remember: in order to justify a reassessment of CHC eligibility, the ICB must demonstrate a significant change in need. If nothing has changed, CHC must continue!
We can provide expert advocacy at the CHC Review.
How to ensure you are properly assessed
You can of course deal with the NHS yourself. Make sure you familiarise yourself with the National Framework and Decision Support Tool.
We have also produced our Free Guide to CHC Funding to help you understand how the process works which you can download for FREE.
Clients often tell us that the Full Assessment is intimidating, stressful and emotionally draining. Sadly, we also hear that some MDTs fail to adhere to the National Framework, or use tactics to minimise the person’s needs.
Our team of qualified CHC Nurse Assessors can provide expert MDT Advocacy at short notice. If you need help, get in touch today.